Mastitis is a common maternal complication experienced by breastfeeding mothers and refers broadly to inflammation of the breast tissues. Up to 30% of lactating mothers experience the early signs and symptoms of mastitis, yet the condition often goes unrecognised, undiagnosed, misdiagnosed, or managed ineffectively. As a result, lactating mothers are frequently given inappropriate advice and as a result, are at a higher risk for weaning before 3 months postpartum.
Mastitis has long been thought of as a single-pathological entity in the lactating breast, with the standard advice being to “heat, rest, and empty the breast”. However, in their recent 2022 review, the America Academy of Breastfeeding Medicine found that Mastitis actually encompasses a range of conditions (best thought of as a spectrum) that result in inflammation and edema (swelling) of the breast tissues. When we consider how inflammation occurs in the body, it stands to reason that heat and emptying the breast may indeed be counter-productive to tissue healing, instead resulting in increased blood flow and milk production to already inflamed breast tissues.
The Mastitis Spectrum
The are multiple factors that contribute to the development of Mastitis including
- Hyperlactation (oversupply)
- Mammary dysbiosis: also known as disruption of the milk microbiome due to
- Exposure to antibiotics, and probiotic use
- Regular use of breast pumps
- Caesarean births
- Maternal genetics and medical conditions
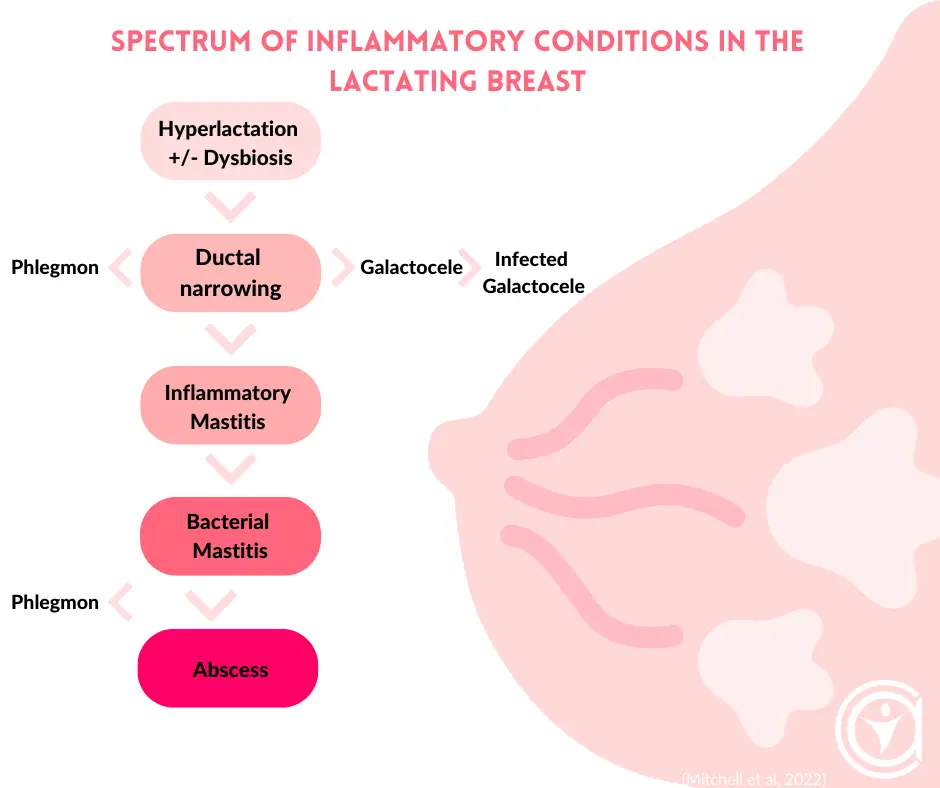
Ductal narrowing
Inflammation and narrowing of the ducts can result in a specific area of thickening/hardening of tissues (induration) and tender, congested breast tissue. There may be mild redness due to lymphatic congestion, but there are no associated systemic (flu-like) symptoms often seen with bacterial mastitis. Mothers should be careful not to aggressively massage their breasts to “remove the blocked duct” as they may cause further tissue damage and progression of mastitis.
Inflammatory Mastitis
The ductal narrowing worsens the inflammation progresses, resulting in increased redness of the breast tissue, swelling, and pain. Systemic signs such as fevers, chills and elevated heart rate may or may not be present. Note: this systemic inflammatory response syndrome may occur in the absence of infection, and may account for an incorrect antibiotic prescription.
Bacterial Mastitis
It occurs with the progression of ductal narrowing and inflammatory mastitis and presents as Cellulitis. Bacterial Mastitis requires treatment with antibiotics or probiotics if symptoms of fever and an elevated heart rate persist for more than 24hrs.
It is not caused by:
- Candida
- Poor breast pump hygiene,
- The inward (retrograde) spread of bacteria due to nipple trauma
Bacterial Mastitis is not contagious and therefore mothers should be encouraged to continue to breastfeed their child throughout mastitis.
Phlegmon
Fluid collections can develop when inflammation is present, often as a result of deep massage which increases edema and causes microvascular injury.
Abscess
Occurs in 3-11% of women with acute mastitis, when either bacterial mastitis or phlegmon progress to an infected fluid collection requiring drainage.
Galactocele and infected galactocele
Occur when ductal narrowing obstructs the flow of milk and causes the milk to collect in a cyst-like cavity, which fluctuates in size throughout the day and with feeds, and can range from 1cm to >10cm.
Recurrent Mastitis
Recurrent symptoms of +/- breast pain, redness, fever, and swelling every 2-4 weeks
Subacute Mastitis
Often follows a history of acute bacterial mastitis. Patients exhibit needle-like burning breast pain, nipple blebs, induration or congestion, and hyperlactation (oversupply).
Mastitis Spectrum-wide management
- Most cases of inflammatory mastitis resolve completely without the need for antibiotics or other interventions.
- It is not usual for a lactating breast to feel lumpy and even painful at times, this doesn’t mean there is necessarily a problem.
- Feed the child on demand, and do not aim to empty the breasts.
- Ice: every hour for comfort (frozen peas work well), do not use cabbage leaves as they have not been shown to be any more beneficial than ice and may carry Listeria bacteria.
- Manual Lymphatic drainage techniques and gentle compressions can assist with fluid drainage.
- Minimise the use of a breast pump.
- Avoid the use of nipple shields.
- Wear a supportive and well-fitted bra.
- Avoid deep massage of the breast tissue, though light, gentle massage using a cold massage ball (Eg. Lactamo) may be of assistance.
- Avoid breast soaks of saline, castor oil and other topical applications.
- Don’t routinely sterilise pumps and household items (eg toys/teethers)
- Decrease inflammation and pain:
- Ice: every hour
- Non-steroidal anti-inflammatories (NSAIDs): Ibuprofen up to 800mg every 8 hrs in the acute phase (check with your GP first)
- Analgesia: Paracetamol up to 1000mg every 8 hrs in the acute phase (check with your GP first)
- Sunflower or soy-lecithin 5g-10g/day oral (to reduce the viscosity of milk)
- Milk blebs: do not debride without consultation with an IBCLC or your GP, use oral lecithin and see your GP for topical steroid cream (1% triamcinolone)
- Reduce oversupply (see a Lactation Consultant (IBLBC) for assistance)
- Therapeutic Ultrasound: to reduce inflammation and relieve oedema, see a qualified health practitioner for use on a daily basis until relief is achieved.
- Only use antibiotics for bacterial mastitis. Incorrect use in cases of inflammatory mastitis disrupts the milk microbiome and can contribute to the progression of bacterial mastitis.
- Probiotics: may be beneficial in the prevention and treatment of mastitis (specifically the Limosilactobacillus fermentum, or Ligilactobacillus salivarus strains. We recommend Qiara.
- Seek support for perinatal mood and anxiety disorder if you are experiencing symptoms. Unsure if you are? Take the PND questionnaire here, and speak with your GP or CFHN.
Therapeutic Ultrasound
Recent studies have demonstrated that Therapeutic Ultrasound may be an effective treatment for mastitis spectrum conditions.
- Thermal and non-thermal effects include the acceleration of metabolic rate, a reduction in pain, and an increase in circulation.
- Method:
- Frequency 1mHz
- Intensity: 2.0W/cm2
- Time: 5 – 6.5mins for an area 2-3x the head of the probe
- Interval: daily
- Resolution usually occurs within 1 week
Lymphatic drainage
Reduces swelling by assisting the movement of lymph fluid, reducing swelling and softening fibrotic tissues.
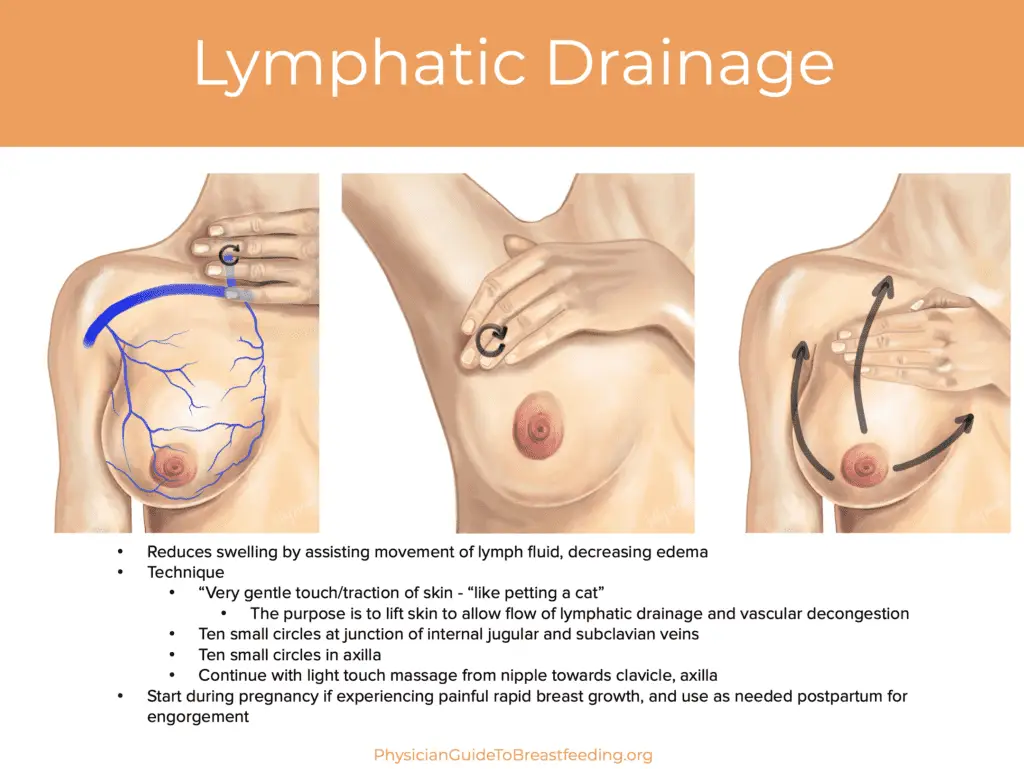
If you prefer a visual demonstration watch this video from Dr. Katrina Mitchell https://youtu.be/-0Uwx7L47cg
To summarise
- Use the principles of inflammation management = Ice, NSAIDs, and physiological breastfeeding
- Address maternal factors: address oversupply, correct milk microbiome, minimise pumping and avoid the use of nipple shields
- Use of gentle lymphatic drainage techniques (practitioner and self-directed) and Therapeutic Ultrasound.
Our team of qualified Osteopaths and Lactation Consultants (IBCLCs) at Completely Aligned are available to assist you with hands-on treatment, therapeutic ultrasound, exercises, and breastfeeding advice/support today. We offer same-day appointments whenever possible for acute cases of Mastitis. You can book an appointment online however for acute cases we encourage you to call us at 02 4655 5588 and let our receptionist know that your GP has referred you, or that you may be experiencing Mastitis and we’ll do our best to assist you, and your baby with your feeding journey today.
References:
Schwartz, K., D’Arcy, H. J., Gillespie, B., Bobo, J., Longeway, M., & Foxman, B. (2002). Factors associated with weaning in the first 3 months postpartum. Journal of Family Practice, 51(5), 439-444.
Scott, J. A., Robertson, M., Fitzpatrick, J., Knight, C., & Mulholland, S. (2008). Occurrence of lactational mastitis and medical management: a prospective cohort study in Glasgow. International breastfeeding journal, 3(1), 1-6.
Mitchell, K. B., Johnson, H. M., Rodríguez, J. M., Eglash, A., Scherzinger, C., Zakarija-Grkovic, I., … & Academy of Breastfeeding Medicine. (2022). Academy of Breastfeeding Medicine Clinical Protocol# 36: The Mastitis Spectrum, Revised 2022. Breastfeeding Medicine, 17(5), 360-376.
Mitchell, K. (2022). Breastfeeding Massage for Lactation: Tips for Clogged Ducts, Lumps and Engorgement. Physician Guide to Breastfeeding. https://physicianguidetobreastfeeding.org/mythbusters/breastfeeding-and-massage/







