Articles by the Completely Aligned team
We believe in producing high-quality healthcare articles sharing our knowledge and experience physical and mental wellness with you so you can learn more about how to live a healthier life.
Browse our healthcare articles below. Feel free to contact us if you have any questions.
Healthcare articles
Explore all our healthcare articles

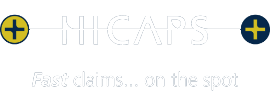
Been Told You Need a Hip Replacement?
July 1, 2024
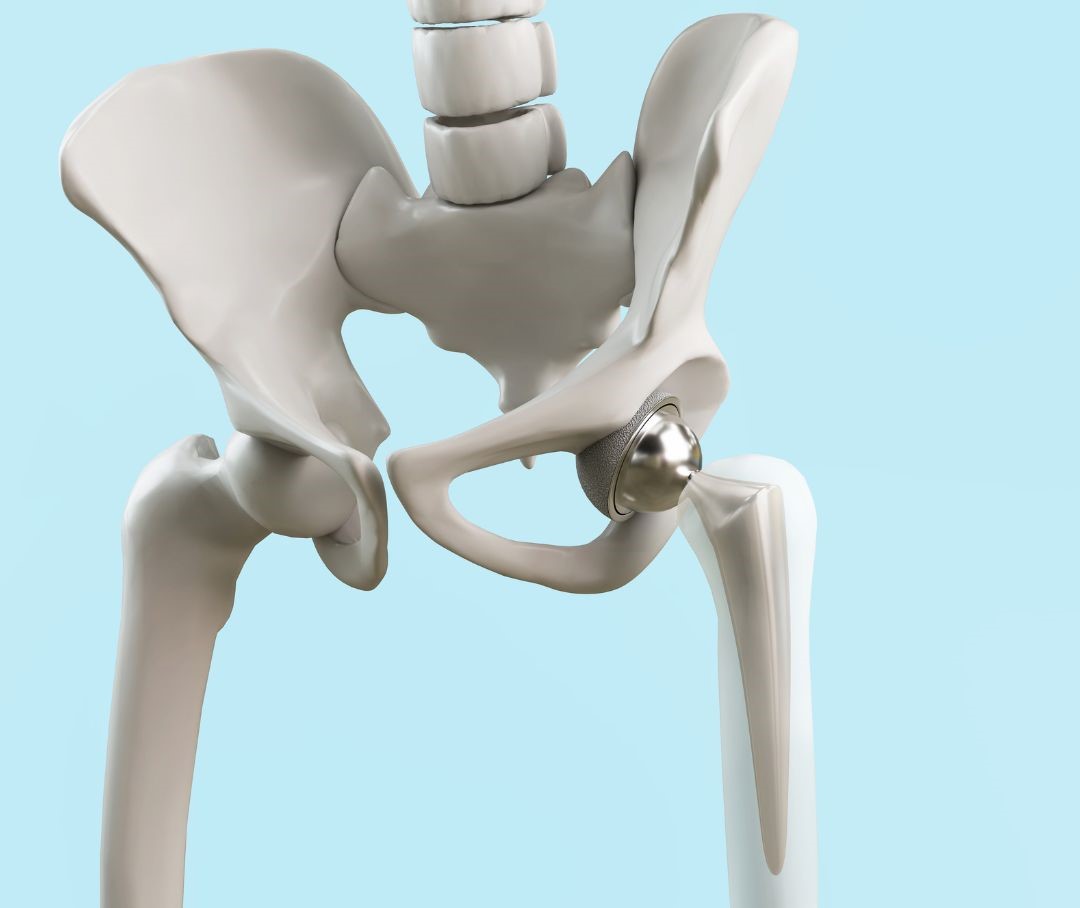
Joint Cracking – An Osteopaths Perspective
June 14, 2024

How Osteopathy Can Help You Recover after a Fracture
May 29, 2024


Increase Shoulder Stability Through Exercise
April 22, 2024

All About Disc Injuries:An Osteopath’s Perspective
April 3, 2024

Lymphatic drainage massage
March 3, 2024

Juvenile Idiopathic Scoliosis:
February 19, 2024
Healthcare guides
Free Downloadable Guides

Setting up your Home Office: an ergonomic how-to guide
Setting up your car: an ergonomic how-to guide

How to pick the perfect pillow
Immune boosting diet

Safely exercising after birth
We're ready when you are
Don't let pain hold you back from doing the things you love
At Completely Aligned, our door is always open for you to get back to doing the things you love in life. Our team are available now to chat with you and work out how we can best support you.